Pott’s Disease: What Is It?
Other names for Pott’s Disease include spinal TB and tuberculosis spondylitis. It is a rare form of TB that affects the spine and is often brought on by an infection from another location.

Multiple vertebrae are affected by osteomyelitis and arthritis, which is how this illness manifests. The lower thoracic vertebrae are most frequently affected, and it typically affects the anterior section of the vertebral body.
When this condition affects the anterior vertebrae, the anterior wedging promotes vertebral collapse, which results in the spinal deformity known as kyphosis (hunched back). Compression fractures, spinal abnormalities, and neurological symptoms, such as paraplegia, are some of the additional complications. The ailment was first identified by Dr. Percivall Pott in the 1700s, and the disease bears his name.
Why Does Pott’s Disease Occur?
The pathogenic bacteria Mycobacterium tuberculosis, which mostly affects the lungs, is what causes tuberculosis. If prompt treatment is not given, it could advance fast to the spine and lead to arthritis. The spinal disc may deteriorate if the infection spreads to two other joints and treatment is delayed because it is receiving fewer nutrients.
The spinal cord is harmed as a result of disc collapse. If treatment is not received, it leads to spinal abnormalities, paralysis, and nerve damage. Only one to two percent of patients who have pulmonary (lung) tuberculosis go on to acquire Pott’s disease.
What Are Pott’s Disease’s Symptoms?
The cervical spine (10%), atlantoaxial area (1%), and lower thoracic vertebrae (40–50%) are the most often affected vertebrae in order.
Primary Signs:
- soreness and tenderness in the area that is afflicted.
- muscular spasm in the related muscles.
- Motion in the spine could become limited.
- spine malformation.
- a neurological disorder.
Back discomfort is by far the most prominent sign of Pott’s illness. Before the patient seeks medical attention, the back pain persists for weeks or even months and manifests as spinal or radicular discomfort. 80% to 90% of spinal tuberculosis sites are located in the thoracic and lumbar spinal regions, which are approximately equally affected. The prevalent site of involvement, however, is most frequently reported to be in the thoracic region of the spine.
About 50% of instances involve neurologic abnormalities, such as compression of the spinal cord and:
- a diminished sense.
- Paraplegia.
- root discomfort in a nerve.
- Cushing’s syndrome.
- Paresis.

Nearly all Pott’s disease patients exhibit spinal deformity. Thoracic kyphosis is the most typical form of spinal deformity.
Additionally Related Symptoms:
- Fever.
- Loss of weight.
- Sweats during the night.
- Malaise.

Cervical spine tuberculosis, a less frequent form, affects 10% of patients. However, due to the severe neurological consequences, stiffness and pain in the neck, torticollis, and hoarseness, this variation is comparatively more severe. The symptoms of upper cervical spine involvement might start off suddenly and progress quickly. The neurological symptoms might range from a single nerve palsy to quadriplegia or hemiparesis along with a retropharyngeal abscess. Patients who have had lower cervical spine injuries may exhibit dysphagia or stridor.
Pott’s Disease in HIV-Infected Individuals:
Human immunodeficiency virus (HIV)-positive individuals are more likely to develop spinal TB, and their clinical symptoms are comparable to those of HIV-negative individuals.
Apparent Population:
In 62% to 90% of those who have the disease, Pott’s disease is asymptomatic, and no extraspinal TB is visible either. This makes timely diagnosis more difficult and makes the prognosis worse.
How is Pott’s illness identified?
The following examinations assist in identifying Pott’s disease:
1) The Mantoux Test (tuberculin skin test):
It is a skin test that uses an injection of a pure protein derivative (PPD) to identify tuberculosis.
2) ESR (erythrocyte sedimentation rate):
It is possible for the erythrocyte sedimentation rate to significantly increase (to more than 100 mm/h).
3) Isolation of the bacteria:
To stain for acid-fast bacilli (AFB), bone tissue samples are obtained. Then, the organisms are isolated for culture and susceptibility testing. Only around 50% of the samples tested positive for the bacterium, though.
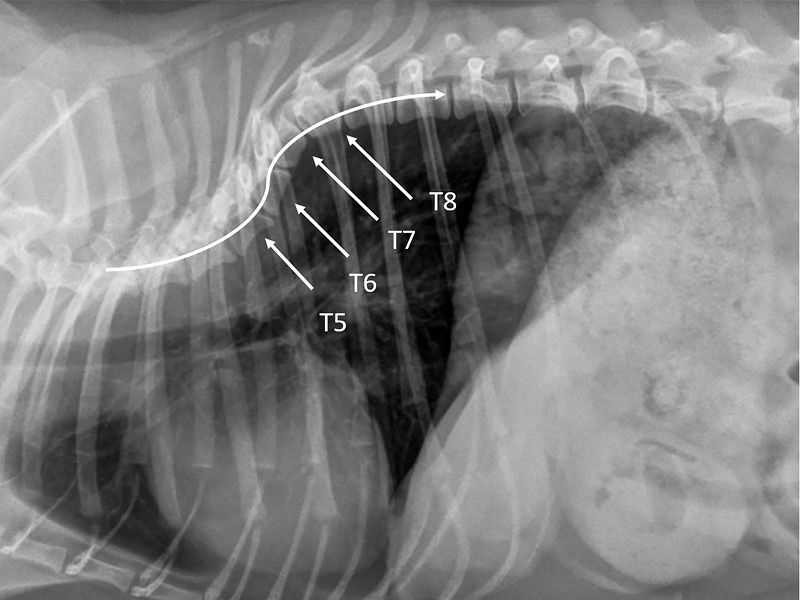
4) Radiographic Modifications:

Typically, the radiographic alterations appear considerably later than the other symptoms. It is possible to see the following changes in plain radiography:
The anterior part of the vertebral body has been destroyed by lytics.
- Progressive lytic reaction-induced sclerosis.
- increased wedging in the anterior.
- the vertebral body collapsing.
- Osteoporotic vertebral endplates are possible.
- expanded psoas shadow, either calcified or not.
- Vertebral bodies exhibit varying levels of deterioration.
- The intervertebral disks may contract or rupture.
- Bone lesions can develop at different levels.
- Fusiform paravertebral shadows indicate the development of an abscess.
5) Computerized Tomography (CT) Scan:
The epidural and paraspinal soft tissues can be evaluated better with low-contrast CT scanning. Additionally, a CT scan reveals sclerosis, disruption of bone circumference, irregular lytic lesions, and disk collapse in the bony detail.
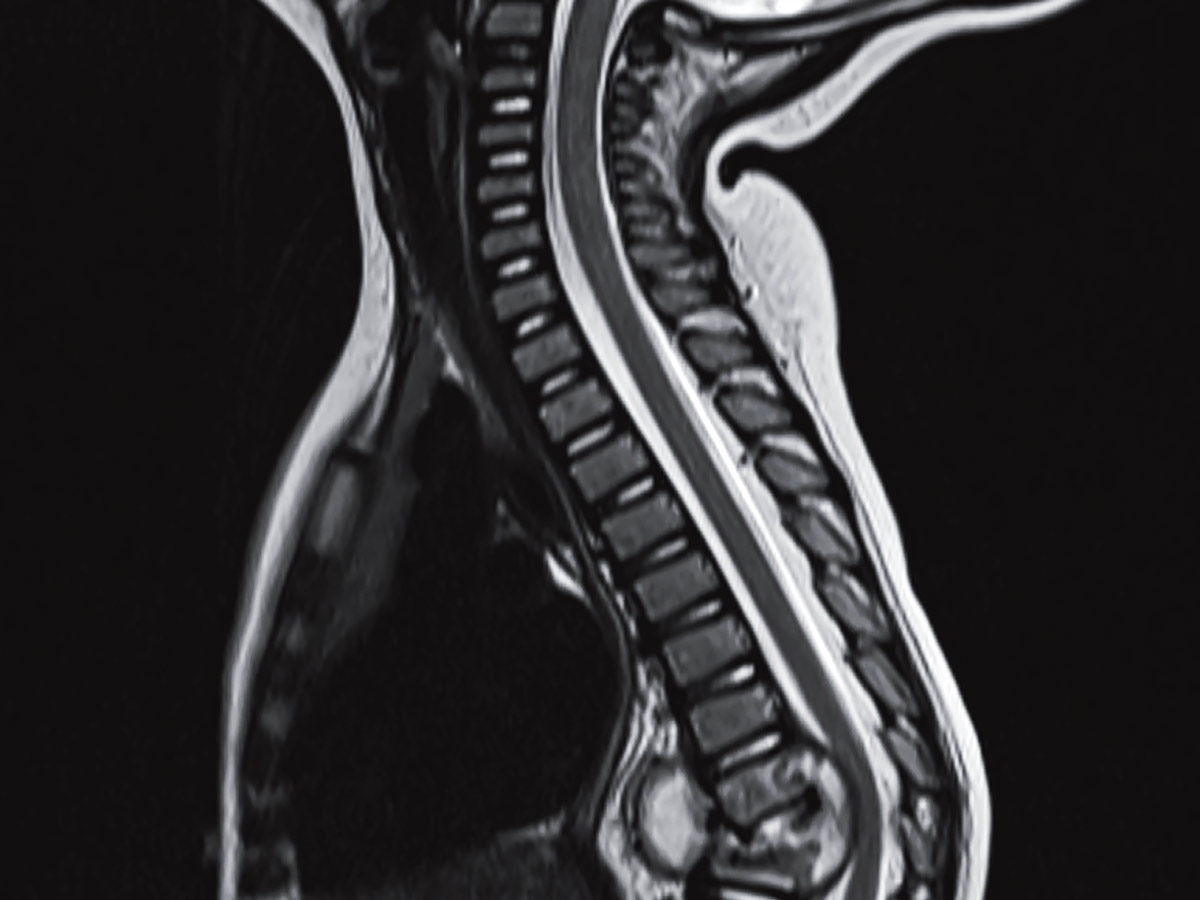
6) MRI stands for magnetic resonance imaging:
MRI is the best diagnostic tool for disc-space infections, neural compression, TB spondylitis (distinguishes from pyogenic spondylitis), and spinal osteomyelitis. It is the most effective in showing how tuberculosis has spread into soft tissue. Additionally, it shows how the anterior and posterior longitudinal ligaments are affected by tuberculosis.
7) Biopsy:
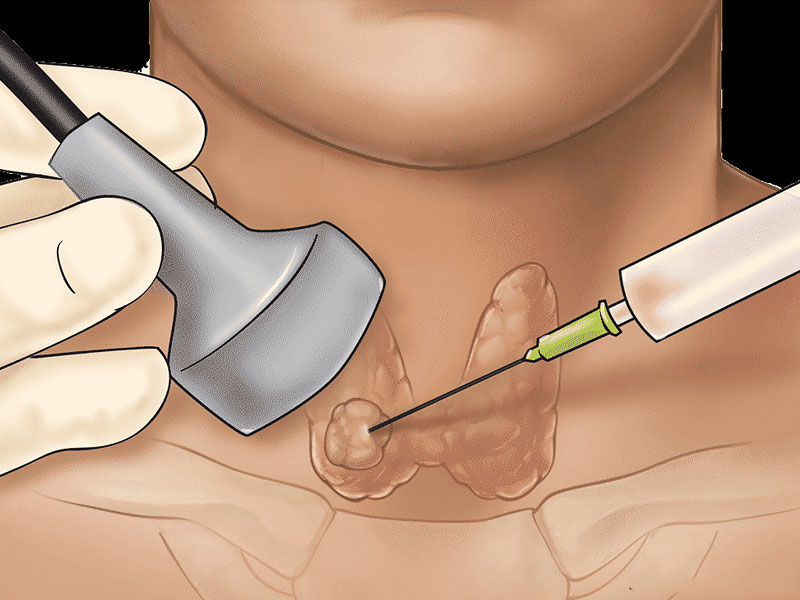
Large paraspinal abscesses can be drained and bone lesions can be sampled using a CT-guided needle biopsy.
8) PCR, or polymerase chain reaction:
Without the requirement for extensive culture, PCR techniques quickly reveal discrete genetic changes in deoxyribonucleic acid (DNA) sequences linked to medication resistance. They are also utilized to diagnose many Mycobacterium strains.
Also, Read Gua Sha – Botox Of The East, Chinese Medicine Of Eternal Youth
Exactly how is Pott’s disease treated?
Each patient’s Pott’s disease therapy is unique and depends on the doctor’s judgment. The average length of the therapy program is between six and twelve months. The prescription drugs work to stop Mycobacterium TB from growing and spreading. Isoniazid and Rifampin make up the initial line of treatment. Throughout treatment, these medications are given. Pyrazinamide, Ethambutol, and Streptomycin are other medications that could be prescribed during the first two months of treatment.

The second line of medications should not be used if there is drug resistance. Despite the effectiveness of pharmaceutical therapy, some conditions necessitate surgical management to stop the disease’s progression and to rectify any abnormalities.
Conclusion:
The disease frequently advances slowly and lasts for months or years. Early diagnosis of the symptoms and use of the most recent treatment regimens improve the prognosis. But the signs are frequently discovered much later. For those who are at high risk, preventive treatments including receiving the BCG (bacillus Calmette-Guerin) vaccine are preferable.